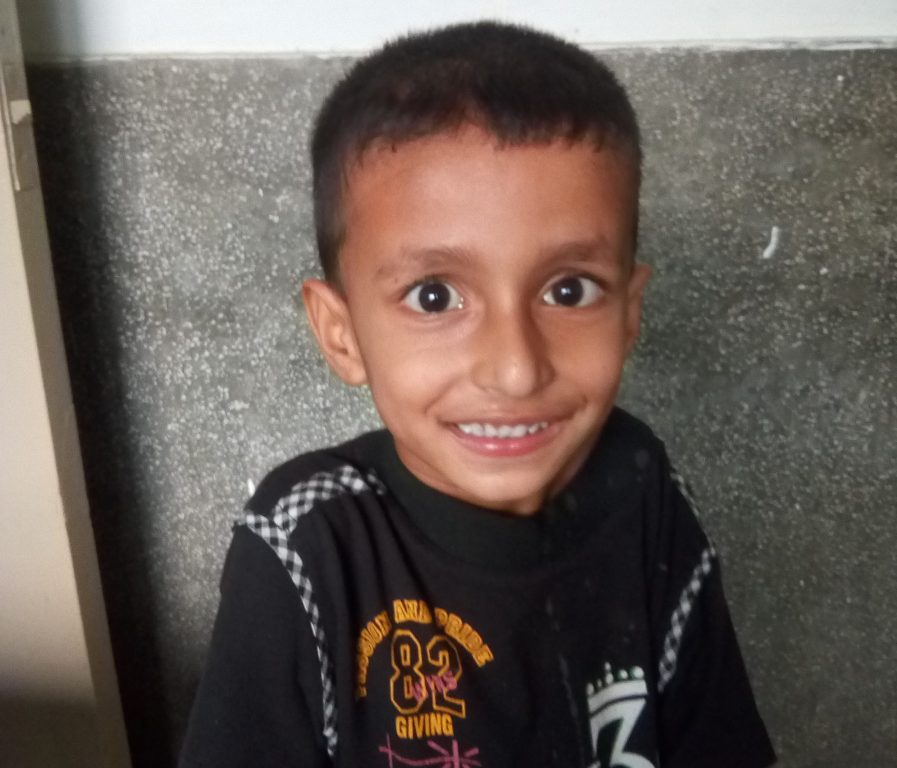
Nepal: Kanti Childrens Hospital
RMF Nurses Triage 787 Patients: Q2 2018
August 01, 2018
Ganesh Shrestha, Pragya Gautam, Dr. Purushottam Adhikari, and Dr. Shreeram Shah
Summary of Activities
Shortly after the April 2015 earthquake, Real Medicine Foundation (RMF) started its support of Kanti Children’s Hospital by donating more than $400,000 worth of medicines, medical supplies, and laboratory supplies. RMF continues to support a blood bank, lodging, food, transportation, medicines, laboratory services, and other necessities for needy patients and their families. In March 2017, RMF also began supporting human resources at Kanti Children’s Hospital and is now providing the hospital with medical officers who serve in the Surgical ICU and Neonatal ICU, as well as registered nurses who serve in the triage area and Medical ward.
April–June 2018
- 7 medical staff members supported by RMF Nepal have continued to serve at Kanti Children’s Hospital.
- 73 patients were treated in the Surgical ICU
- 183 patients were treated in the PICU
- 656 patients were admitted to the Medical ward

Results &
ACCOMPLISHMENTS

ICU
Pediatric and Surgical
RMF’s medical officers served a total of 183 patients at the PICU and 73 patients in the Surgical ICU of Kanti Children’s Hospital from April to June of 2018.
The ICU beds provided by RMF in previous quarters are now fully functioning and being utilized in the ICU.

Emergency Triage
787 Patients
RMF nurses use a triage system while serving in the Emergency Unit of Kanti Children’s Hospital. Through this system, they classify and provide tags to the patients: code red requires immediate medical action for survival, code yellow indicates a serious but not life-threatening condition, code green indicates a less severe condition that can wait, and code black means dead on arrival. In the triage section of the Emergency Unit, patients are sent to the respective color zone for treatment, generally either the red or the yellow zone. From April to June 2018, RMF nurses classified a total of 787 patients with 99 code reds and 688 code yellows.
Medical Ward
656 patients
From April to June of 2018, a total of 656 patients were admitted to and treated in the Medical ward. Among them, 241 patients were female, and 415 were male. The most common systemic disease in the Medical ward was respiratory disease, followed by cardiovascular disease.

Background
& Objectives
Background
Kanti Children’s Hospital is the only government referral level Children’s Hospital of Nepal. The hospital was established in 1963 as a general hospital with 50 beds, which today have a capacity of 320 beds. The hospital treats children up to the age of 14 from all over the country, a total target population of 13-14 million children. Following the earthquake, where parts of hospital building were damaged, there is in general a need for equipment and capacity building for better health service delivery.
Objectives
- Provide necessary medical supplies, blood, and nutritional support for patients. Also providing access and transportation to testing and procedures
- Give instruction of patients needs, education, amenities during hospital stay, and financial support to family of the patient
- Management to various hospital programs such as a blood drive program, a free-of-cost kitchen for patients and families, playroom and library for patients and siblings, and clothes bank for needy patients and family

More
Photos
Click to enlarge





Numbers
Served
Patients Served this Quarter
DEPARTMENT TOTALS
Pediatric ICU-183
Surgical Intensive Care-102
Emergency Unit Triage-633
Medical Ward-639


More Reports on: Kanti Childrens Hospital Archive
Country Page: Nepal
Initiative Page: Kanti Childrens Hospital